Ethosuximide in MDD
Armin Moradi
2020-02-11
Table of Contents
Overview
Introduction
- A new rapid-acting antidepressant akin to ketamine on the rise?
Rationale (why care?)
Ethosuximide
- already widely used as anticonvulsant agent
- known and better side-effect profile vs ketamine and esketamine
- rapid antidepressant action in rodents
- potential for use in treatment-resistant MDD (both es/ketamine)
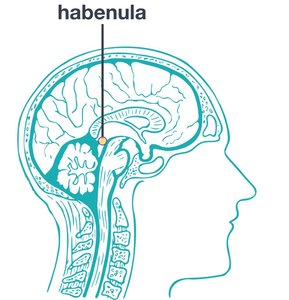
Lateral Habenula
Rationale (but…how?)
- Lateral Habenula (LHb) burst fire inhibition = rapid-acting antidepressant
- NMDA + T-VSCC = burst fire
- A AND B = C -> inhibit A OR inhibit B = inhibit C
Primary Goals
- Is ethosuximide any good for depression?
Methods
- Double-blind
- Randomized
- Placebo controlled
- Three mental health centres in China
- Three different doses
- 80 participants, 4 groups (3 ethosuximide, 1 placebo)
Results
:(
Author's Conclusion
:(
Authors
Funding and Support
- National Nature Science Foundation of China
- Wuxi Technology Bureau
- Wuxi Municipal Health and Family Planning commission
Conflict of interest
One researcher (Dr. K. Hashimoto) has a pending patent for "Application of R-ketamine and salt thereof as pharmaceuticals" by Chiba Univesity, and has received research support by Otsuka, Sumitomo-Dainippon, and Taisho pharmaceutical companies.
Introduction
Background and rationale
- Reference to prior preclinical studies.
- Information regarding the role and mechanism of action of ketamine and its relation to ethosuximide was provided
- Motivation: good parts of ketamine less the bad parts
Hypothesis and research question
- Hypothesis: ethosuximide is efficacious for treatment of MDD in treatment-naive patients
- Objective: to evaluate the antidepressant efficacy of ethosuximide in comparison with placebo in treatment-naive adult patients with MDD
- Primary outcome: HAM-D score change from baseline vs placebo over 5h and 2 weeks
- Secondary outcomes: MADRS/HAM-A/VAS score change from baseline vs placebo over 5h and 2 weeks
Methods
Design
- Multicenter, Double-blind, Placebo-controlled
- First RCT for ethosuximide: no sample size estimation
Recruitment
- Adults 18-65 with confirmed single or recurrent MDD based on MINI
- No information on method of recruitment was provided
- No information on compensation: none?
Screening
- No pre-screening information was provided
Screening
- inclusion criteria
- score of 18 on 17-item HAM-D AND no antidepressant treatments in past 6 months
Screening
- Exclusion criteria
- substance abuse/treatment in previous 3 months
- active suicidal intent
- pregnancy
- bipolar
- psychotic disorder or current psychotic symptoms
- unstable medical illness
- significant neurological illness
- abnormal serologic findings
Participants
- 112 patients assessed, 17 declined to participate, 32 did not meet inclusion criteria
- 80 randomly assigned evenly to 4 groups known only to pharmacy administrators (double-blind)
- Ethosuximide 500mg
- Ethosuximide 1000mg
- Ethosuximide 1500mg
- Placebo
- even distribution
Administration
- Each group has x1 dose on first day of treatment
- 1500mg and placebo groups had repeat dose daily for 2 weeks
- Timing of doses in the day, preparation of oral medication (pill, tablet, liquid, gel, etc.) not discussed
Assessment
- HAM-D and MADRS were used for scoring
- Visual Analog Scale (VAS) was used to monitor dependent symptoms
- HAM-D, HAM-A, MADRS, and VAS were administered at 1h and 5h after single dose oral administration
- for repeat group, HAM-D, MADRS, HAM-A, and VAS were measured at
- baseline
- end of first week
- end of second week
Measures
- HAM-D, HAM-A, MADRS, VAS
- General demographics data:
- age
- gender
- years of education
- height
- weight
- length of MDE
Statistical Analysis
- data collected as means +/- std deviation
- Baseline characteristics compared using Pearson x2 test for categorical variables
- One-way analysis of variance (ANOVA) used for continuous variables
- primary outcome: HAM-D
- secondary outcome: MADRS, HAM-A, and VAS
- changes in baseline in above measures were assessed with repeated measures one-way ANOVAs followed by post-hoc Fisher's least significant difference test
Results
Scores
| Control | 500mg | 1000mg | 1500mg | |
|---|---|---|---|---|
| HAM-D | 25.20 +- 5.75 | 26.15 +- 6.56 | 23.95 +- 4.37 | 26.85 +- 4.06 |
| HAM-A | 10.35 +- 2.18 | 11.30 +- 2.60 | 10.95 +- 2.63 | 10.65 +- 2.01 |
| MADRS | 26.90 +- 5.71 | 28.20 +- 6.84 | 26.00 +- 4.65 | 28.90 +- 4.19 |
Statistical Significant
Primary outcome (HAM-D)
| Time | P-value |
|---|---|
| 5h | 0.243 |
| 2w | 0.263 |
Statistical Significant
Secondary outcome
| Test | Time | P-value |
|---|---|---|
| MADRS | 5h | 0.214 |
| 2w | 0.260 | |
| HAM-A | 5h | 0.425 |
| 2w | 0.824 | |
| VAS | 5h | 0.472 |
| 2w | 0.623 |
Statistical Significant
No significance
Clinical Significance
?
Reliability
- The good
- Primary outcome based on objective measures (HAM-D, HAM-A, MADRS, VAS)
- 100% rate of completion
- Double blind
- Similar groups at the start of the study, treated equally except treatment
- All patients analyzed
- Low (<40%) placebo response
Reliability
- The bad
- Sample size assumed based on animal studies, no statistical analysis
- The ugly
- …
Generally Reliable
Conclusion
Statistical Interpretation
Results indicate that ethosuximide does not have antidepressant actions in non-medicated patients with MDD
- There isn't much room for artistic interpretation
- Both primary and secondary outcomes: large P-value = No significance
- High placebo response
- >40% response muddies the water
- this study -> low placebo response
Limitations
- Only 80 patients -> "preliminary results"
- Needs bigger samples
- Strict inclusion criteria
- "unclear whether findings will generalize to all patients with treatment-resistant MDD."
Conclusion
- No severe adverse events
- Did not mention what adverse events, if any, were reported by patients
- Did not alter VAS score after 2 weeks -> low potential for abuse
Conclusion (2)
- Demonstrated antidepressant effect of ethosuximide in rats with absence epilepsy and comorbid depression-like behaviour
- Also effective in rats subjected to chronic restraint stress
It seems that antidepressant-like effects of ethosuximide are limited to WAG/Rij rats, which suggests a link between absence seizures and depressive-like behaviours in this strain of rats.
Conclusion (3)
- Previous studies failed to produce antidepressant effect in a stress model of chronic social defeat
- R-ketamine did show antidepressant effect
- This study supports the above
Conclusion (4)
We could not find any antidepressant effect of ethosuximide on the clinician-reported HAM-D and MADRS scores after single and repeated oral administration. Therefore, it is unlikely that ethosuximide elicits ketamine-like rapid-acting antidepressant actions in patients with MDD, but the negative findings need to be replicated by other research groups.
Discussion
Interpretation
Results appropriately interpreted
Explanation
- Adequately explained limitations except
- Standardization process among 3 centers
- Medication administration process
- Randomization process (computer? dice? deck of cards?)
Consistent
Consistent conclusion
Generalizable
- Ethnicity was not discussed at all
- HAM-D scores had a relatively low std dev
- Use of ethosuximide in treatment-naive patients is unlikely at this point
Literature correspondence
- R-ketamine vs ethosuximide in rats
Clinical practice
No change at this point
Future
- Ethosuximide in treatment-resistant MDD (under way)
- Bigger sample size
- Different populations (wider range of ethnicities), multinational
- Humans with absence seizure and comorbid MDD
- Targeting other parts of the same pathway (different medications)